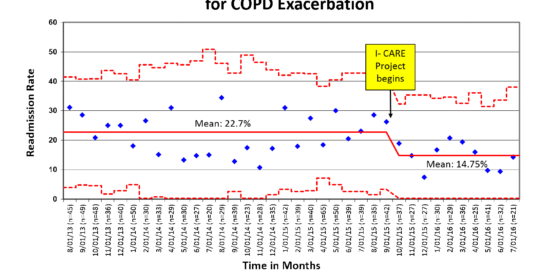
University of Cincinnati Medical Center Reduces Readmissions After COPD Exacerbation by 35%
University of Cincinnati (UC) Medical Center has reduced hospital readmissions in patients with acute exacerbations of chronic obstructive pulmonary disease (AECOPD) by more than 30% over the past eight months. Muhammad Zafar, MD, clinical instructor and medical director of pulmonary rehabilitation at the UC Medical Center, is the head of the quality improvement project, Improving COPD Acute decompensation Readmissions (I-CARE): Best Practice Compliance in In-Patient Setting, which realized these outcomes.
The I-CARE Project has helped reduce COPD readmissions by 35%, through system redesign using improvement science.
Image courtesy of Dr. Muhammad Zafar, MD
As Dr. Zafar explains, in 2010, the cost of COPD care was $50 billion,1 and hospitalizations for AECOPD accounted for more than one-fourth of this cost.2 COPD readmissions after an acute exacerbation have been part of the Medicare Hospitalization Readmission Reduction Program since 2014, resulting in reduced reimbursements under the inpatient prospective payment system.3 More importantly, COPD readmissions affect patients adversely, leading to reduced quality of life and higher risk of death.
In assessing opportunities for improved care for patients with COPD, Dr. Zafar and his colleagues applied improvement science methodologies to redesign the care delivery system in order to minimize errors and failures in patient care. Dr. Zafar focuses on improvement science methodology in his role as Quality Scholar, James Anderson Center for Health System Excellence, Cincinnati Children’s Hospital Medical Center, where he studies the science of human behavior along with other components needed to apply quality improvement methodology to health care systems.
These methodologies, which have been used in industry and production,4 are becoming more commonplace in health care systems. I-CARE’s multidisciplinary effort involves pulmonologists, hospitalists, pharmacists, case managers, respiratory therapists and nurses. “We analyzed our care delivery, performed retrospective chart reviews, examined the literature for guidelines and evidence-based practices and interviewed patients. We looked at patient and system factors to determine where our system was failing to produce consistently applied evidence- and guideline-based care,” he says. In doing so, Dr. Zafar says, everyone developed a better understanding of the existing system, the key staff and processes involved and patient perspectives.
Dr. Zafar’s project identified a five component, best-practice bundle for COPD admissions to mitigate system level failures and provide evidence-based care where it was lacking. The goal was to redesign the multidisciplinary care process in order to reliably deliver all components of the COPD bundle to all patients admitted with AECOPD, hence reducing readmissions. In characterizing the impact of this project at UC Medical Center, Dr. Zafar says that a reliable system of care delivery, with all patients consistently receiving good care, has been established. The system redesign makes it easier for physicians, respiratory therapists, pharmacists, nurses and social workers to provide better care, and makes evidence-based medicine a system property rather than individual responsibility. The majority of system level failures that contribute to readmissions have been mitigated, without adding extra personnel or raising costs. Finally, care has become patient-centered in its true sense, for the benefit of those we serve.
Dr. Zafar is proudest of the impact that I-CARE has had on patients with COPD, who now leave the hospital with the tools and information needed to succeed in managing their condition. In addition to improved patient outcomes, a collateral benefit of doing what is right for patients is that the medical center will achieve a higher hospital rating, and patients, hospitals and insurance companies will save money.
Plans are underway to expand the project to reducing emergency room visits for patients with COPD and other similar pulmonary diseases, such as asthma.
References
1. Guarascio AJ, Ray SM, Finch CK, Self TH. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinicoecon Outcomes Res. 2013;5:235-245.
2. Pasquale MK, Sun SX, Song F, et al. Impact of exacerbations on health cost and resource utilization in chronic obstructive pulmonary disease patients with chronic bronchitis from a predominantly Medicare population. Int J Chron Obstruct Pulmon Dis. 2012;7:757-764.
3. Readmissions reduction program. Centers for Medicare & Medicaid Services. Available at https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Accessed July 25, 2016.
4. Deming, W. Edwards. The New Economics for Industry, Government, Education. 2nd ed. The MIT Press. Cambridge, MA, 1993.
 Muhammad Ahsan Zafar, MD, FCCP
Muhammad Ahsan Zafar, MD, FCCP
Clinical Instructor
Medical Director of Pulmonary Rehabilitation
Pulmonary and Critical Care Medicine
University of Cincinnati
Email: zafarmd@ucmail.uc.edu
Connect with Dr. Zafar on Doximity
Leave a reply →
