Round-the-Clock Medical Intensive Care Unit Coverage by Board-Certified Intensivists Improves Patient Safety
As many as 66% of ICU patients are admitted outside of standard business hours.1 Frequently, multiple pulmonary procedures such as intubations, extubations, and resuscitations need to be performed simultaneously in the ICU. While 24/7 coverage by board-certified critical care intensivists would seem a desirable approach to optimizing ICU safety and outcomes, the debate around cost-effectiveness and direct impact on outcomes continues. Recent high profile studies have failed to show benefit from round-the-clock coverage, yet the lower mortality rates found in major teaching hospital ICUs suggest that in-house physician coverage has an important impact.2
University of Cincinnati Medical Center initiated its own such model three years ago. During the day, two teams cover the 24 ICU patients, and at night an in-house intensivist covers all cases. One study reported a per patient day decrease from 11% to 7% in the rate of intensive care unit complications before and after round-the-clock intensivist coverage was implemented. More than 75% of providers considered the model optimal for patient care.3 University of Cincinnati Medical Center’s nocturnal intensivist program was implemented two years ago and has had an unmistakable impact. In the opinion of Thomas Preston, MD, assistant professor, department of internal medicine, “This model improves physician education for both residents and fellows, benefits the patients by enhancing continuity and safety of care, and buoys the confidence of nurses, respiratory therapists and other staff through more timely and expert interventions.” According to Preston, approximately 80% of MICU patients experience a life-threatening complication requiring high level critical care expertise such as respiratory failure, bleeding or the onset of sepsis, and at least half of those occur in the period between 6 p.m. and 6 a.m.
Prevention of nosocomial infections is a widely accepted quality metric in the ICU. David Norton, MD, Assistant Professor, Department of Internal Medicine and Director, Intensive Care Unit states, “Since the nighttime intensivist program has started, there has been a higher number of extubations and central line withdrawals after hours, which translates to earlier removal of these potential infection pathways and lower rates of nosocomial infections. Indeed, infection rates related to central intravenous lines, ventilators, and Foley catheters have all decreased in the MICU. While this reduction cannot be attributed solely to the 24/7 ICU intensivist model, it has certainly been a significant part of the solution.
The NIH-sponsored Prevention and Early Treatment of Acute Lung injury (PETAL) program seeks to improve outcomes for patients with, or at risk for, Acute Lung Injury (ALI) or Acute Respiratory Distress Syndrome (ARDS). University of Cincinnati Medical Center is one of 19 centers invited to participate in this seven-year study slated to execute three to five prospective, randomized trials.4 In many of these studies, patients need to be enrolled within hours of presentation. The institution’s nocturnal intensivists will assist with recruitment, providing rapid enrollment for studies with narrow recruitment windows.
The benefits of expert, in-house, nocturnal ICU care are hard to prove in controlled studies, but are readily apparent to those who have practiced in ICUs before and after the implementation of round-the-clock programs. Concludes Norton, “For large, high-complexity ICUs offering state-of-the-art care and cutting-edge research, I believe 24/7 intensivist coverage is not just the future, but the ‘now.’”
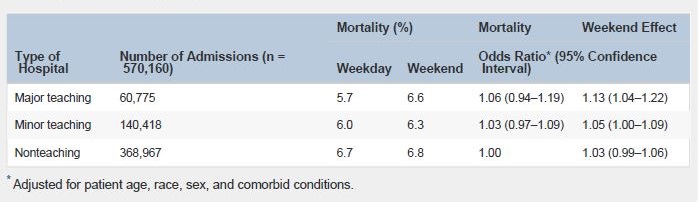
Number of Admissions and Risk-Adjusted In-Hospital Mortality among Patients Admitted to Major Teaching, Minor Teaching, and Nonteaching Hospitals2
David Norton, MD
Assistant Professor, Department of Internal Medicine
Director, University of Cincinnati Medical Center Intensive Care Unit
Medical School: University of Virginia School of Medicine
(513) 558-4831
david.norton@uc.edu
 Thomas Preston, MD
Thomas Preston, MD
Assistant Professor, Department of Internal Medicine
Medical School: Ohio State University College of Medicine
(513) 558-4831
prestots@ucmail.uc.edu

