
If Poorly Controlled Asthma is Suspected, Consider Excessive Dynamic Airway Collapse (EDAC)
In a new program at the University of Cincinnati (UC) Medical Center, patients who have a presentation consistent with poorly controlled asthma are undergoing testing to determine if they actually have excessive dynamic airway collapse (EDAC) instead. EDAC is a common condition in which the soft tissue of the posterior wall of the trachea bulges forward and touches the anterior wall during tidal breathing. The condition often occurs in association with tracheomalacia, in which cartilage in the trachea loses its rigidity and becomes floppy. Together these processes result in airway obstruction during exhalation that can mimic more common obstructive lung diseases.
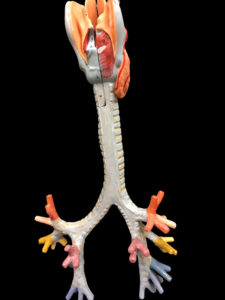
Proximal tracheobronchial tree, shown from the posterior view to demonstrate the relationship between the posterior membrane that becomes ‘too floppy’ in EDAC, and the tracheobronchial cartilaginous rings, which are structurally weakened in patients with bronchomalacia. Image courtesy of Julian Guitron, MD.
Sadia Benzaquen, MD, associate professor of medicine and director of interventional pulmonology, and Julian Guitron, MD, assistant professor of surgery, are directing efforts to identify patients who may have EDAC. Dr. Guitron explains that “the symptoms of EDAC are not very different from those of poorly controlled asthma, such as coughing, wheezing, shortness of breath, and chest tightness.” Often these patients are started on medications, such as steroids, which exacerbate EDAC. Steroids result in weight gain, which worsens both EDAC and gastric reflux. Many investigators believe that reflux from the stomach causes softening of the airways over time, contributing to the development of EDAC.
UC Medical Center established a comprehensive airway tracheomalacia program to treat patients with EDAC, as well as tracheomalacia, about 18 months ago. “Patients undergo extensive testing to confirm an EDAC diagnosis and determine if they will benefit from surgery,” says Dr. Guitron. “GI testing is an essential component of the work-up that is too often over-looked by other centers”.
Dr. Guitron estimates that only one of ten patients referred for evaluation of refractory airflow obstruction is found to have EDAC. Of the 30 patients assessed in the last 18 months, two patients were considered eligible for surgery; a two-step process that includes insertion of a Y-stent, followed by a tracheobronchoplasty. The Y-stent is a silicone tube fitted to match the size of the patient’s windpipe. “Implanting the Y-stent provides temporary support to the windpipe and allows us to determine if the patient will respond to a tracheobronchoplasty,” Dr. Guitron says. The Y-stent is removed after a therapeutic trial spanning several days, and a tracheobronchoplasty is peformed two weeks later, when inflammation has resolved. “We tighten the trachea wall and place a permanent mesh on the entire, cranio-caudal expanse of the tracheo-bronchial tree that is accessible in the surgical field,” Dr. Guitron says .
The multidisciplinary team, involving interventional pulmonologists, thoracic and general surgeons, and social workers, meets regularly to discuss patients, assess candidacy for surgery, and track outcomes. Patients who have undergone tracheobronchoplasty thus far have had excellent results based on the improvement or resolution of symptoms that leads to improved quality of life, Dr. Guitron says . Dr. Benzaquen and Dr. Guitron are establishing a database to track outcomes for both surgery and non-surgery eligible EDAC patients.
The University of Cincinnati welcomes referrals of patients with refractory airflow obstruction for evaluation of EDAC.
 Sadia Benzaquen, MD
Sadia Benzaquen, MD
Associate Professor, Medicine
Director, Interventional Pulmonary
Phone: 513-558-4831
Email: sadia.benzaquen@uc.edu
Connect with Dr. Benzaquen on Doximity
 Julian Guitron, MD
Julian Guitron, MD
Assistant Professor of Surgery
Phone: 513-584-1387
Email: guitrojn@ucmail.uc.edu
Connect with Dr. Guitron on Doximity
Leave a reply →
