How does COVID-19 affect the overall respiratory system: short and long term?
COVID-19 can affect the respiratory system in a variety of ways and across a spectrum of levels of disease severity, depending on a person’s immune system, age and comorbidities. Symptoms can range from mild, such as cough, shortness of breath and fevers, to critical disease, including respiratory failure, shock and multi-organ system failure.
It is particularly important that patients who have underlying lung disease can certainly have worsening of those conditions with contraction or exposure to COVID-19. With this, COVID-19 can cause overall worsening of these conditions, such as asthma, chronic obstructive pulmonary disease (COPD), interstitial lung disease, etc.
For those people who are diagnosed with COVID-19 and then recover, what are the short-term effects of COVID-19 on the lungs?
According to the World Health Organization, recovery time appears to be around two weeks for mild infection and three to six weeks for severe disease. However, this is variable and depends on a patient’s pre-existing comorbidities in addition to illness severity.
Several surveys conducted in the U.S. and Italy are showing that only 39% of those who had been hospitalized reported a return to baseline health by 14-21 days after diagnosis.
Similarly, in a study of 143 patients hospitalized for COVID-19, only 13% were symptom-free after a mean of 60 days following disease onset.
The most common symptoms were dyspnea (43%), fatigue (53%), joint pain and chest pain.
However, there have been reports of persistent severe illness with weeks of fevers and pneumonia persisting in immunosuppressed patients.
With milder infection, patients can still have prolonged symptoms. A recent survey showed that only 65% reported a return to baseline health by 14-21 days after diagnosis. Those who did return to baseline health did so a median of seven days after the diagnosis. Symptoms that can persist include cough (43%), fatigue (35%) and rarely fevers and chills in those with prior mild infection.
What are the physiological changes in lung structure and function that causes serious complications? What causes these changes specifically?
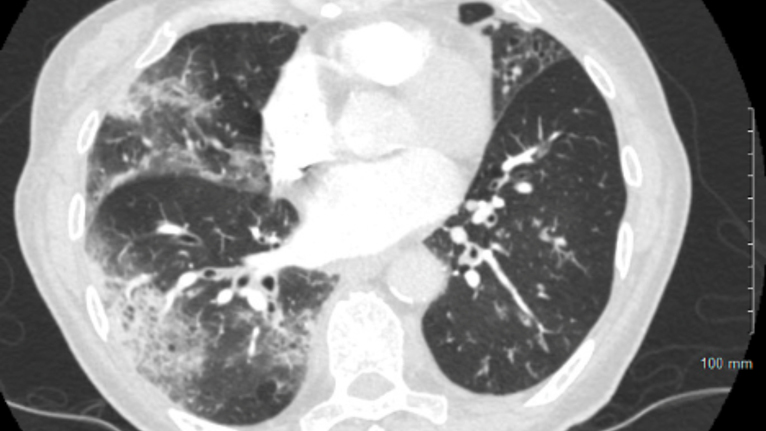
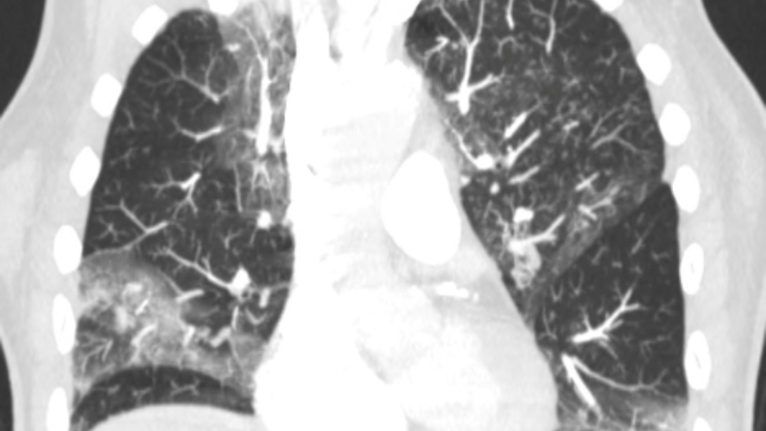
A major issue with COVID-19 is with gas exchange in the alveolus. Usually, there is a very tight connection between the alveolar epithelium (type-1 cells) and the capillary. COVID-19 infects AT2 cells, kills them and floods the alveolus. In addition, there is evidence for microthrombosis, which may block the vascular side.
Clinically, this may appear as several conditions: severe bronchopneumonia, acute respiratory distress syndrome (ARDS) or sepsis.
Pneumonia is inflammation and fluid in the lungs, making it difficult to breathe. Patients can experience shortness of breath, fevers and cough, which can be productive. More severe inflammation can lead to ARDS, which can require significant treatment including the use of oxygen therapies, including mechanical ventilation or even extracorporeal membrane oxygenation (ECMO), which is a lung bypass machine that oxygenates the blood. If a patient develops this severe of a syndrome, this can lead to longer-lasting effects on the lungs, such as fibrosis (scarring of the lung).
Sepsis is a syndrome of abnormal inflammation that usually results from infection. It can lead to multiple organs not working in a coordinated fashion. This syndrome can require support for failing organs, and thereafter, have a lasting impact on their long-term functionality.