Cardio-oncology Program Launches Multi-Pronged Approach to Understanding, Treating, and Preventing Cardiotoxicity in Cancer Patients
The University of Cincinnati Medical Center is preparing to formally launch a Cardio-oncology Program, in response to substantial unmet needs to mitigate risk of acute and delayed cardiomyopathy resulting from cancer treatment. According to Richard Becker, MD, division chief of cardiovascular health and disease and physician-in-chief, University of Cincinnati Heart, Lung and Vascular Institute, “We’re well aware of the risks for acute cardiotoxicity during chemotherapy, such as with anthracyclines like doxorubicin, or with exposure to radiation treatment that can be quite serious.1 But delayed toxicities, particularly atherosclerosis, systolic dysfunction and aortic aneurysms, sometimes decades after chemotherapy, have more recently come to light.2 These findings highlight the progress that has been made in the treatment of patients with cancer; however, in many cases the mechanisms underlying cardiotoxicity are simply unknown.”
Cardio-oncology is an emerging field that formally approaches the study and clinical treatment of cardio-toxicity in cancer patients. The cardio-oncology program at the University of Cincinnati Medical Center and Center for Rare Cardiovascular Diseases and Conditions within the Heart, Lung and Vascular Institute represents a collaboration of adult cardiology experts such as Becker and David Feldman, MD, pediatric heart specialists such as John Lynn Jefferies, MD, MPH, in the Heart Institute at Cincinnati Children’s Hospital Medical Center and William Barrett, MD, Director of the University of Cincinnati Cancer Institute. A key aspect of the program will be to better understand the development of both acute and delayed cardiomyopathy, based not only on preclinical research, but also longitudinal study of pediatric and adult patient cancer survivors.
The multipronged effort will also include educational and clinical components. Cardiology fellows will spend time with the cardio-oncology unit, with the ultimate goal of a separate fellowship program in this emerging subspecialty. Becker notes, “As part of this program, we also intend to implement institution-wide screening and treatment protocols designed to identify oncology patients at risk for cardiotoxicity, to detect early signs of cardiotoxicity, and take preventive steps to minimize cardiac risks.” This will include the use of scheduled echocardiography, blood tests for biomarkers of cardiotoxicity such as troponins, as well as DNA samples to identify genetic risk factors.
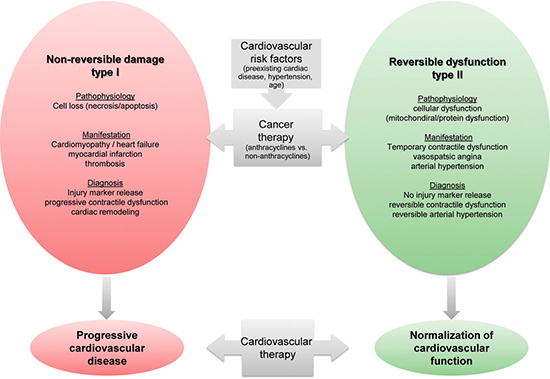
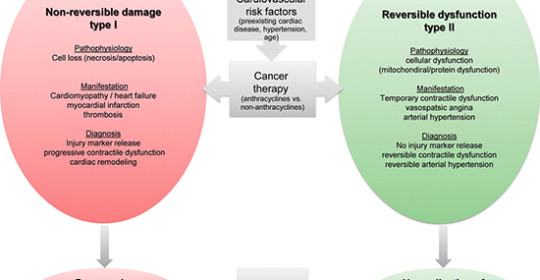
Image courtesy of T.M. Suter & M.S. Ewer Cancer drugs and the heart: importance and management. European Heart Journal, 2012, Jul 12 08:04, 3.
Becker adds, “While there are currently no drugs known to protect the heart against chemotherapeutic cytotoxicity, certain steps may minimize the risks. In addition to monitoring patients for toxicity, physicians can avoid the use of risky chemotherapeutic dose schedules or combinations, carefully observe dosing limits, and can shield the heart during radiation treatments. Physicians can also consider using alternative chemotherapies in patients with heart disease risk factors or pre-existing comorbidity.”
Because some cardiotoxicity symptoms, such as fatigue, malaise, and shortness of breath, can be difficult to differentiate from other chemotherapy side effects, Becker plans that a multidisciplinary team, which includes a cardiologist, will assess oncology patients on a case-by-case basis, as he explains, “To help tease out possible cardiotoxicity from other conditions that commonly occur in these patients.” As the program takes its first steps in 2015, it promises to raise awareness among physicians of cardiac risks for all cancer patients, setting in motion substantive changes to care in the years ahead.
 Richard C. Becker, MD
Richard C. Becker, MD
Mabel Stonehill Endowed Professor of Medicine
Chief, Division of Cardiovascular Health and Disease
Director and Physician-in-Chief
University of Cincinnati Heart, Lung and Vascular Institute
University of Cincinnati College of Medicine
Director, Cardiovascular Services
(513) 558-4332
beckerrc@ucmail.uc.edu

