Novel MRI Approaches Provide Risk-free High Resolution Images of Lung Structures
“Most of us were taught that magnetic resonance imaging (MRI) is not useful for studying the pulmonary parenchyma; but that is changing,” says Frank McCormack, MD. Jason Woods, PhD, agrees that use of MRI in pulmonary disease is coming of age, as clinicians learn that novel MRI approaches can provide risk-free high resolution images of lung structures, a method to quantify regional ventilation1 and information about alveolar/airspace size2 that are not available by any other technology, including computed tomography (CT). Dr. McCormack is professor of medicine and director of the division of pulmonology, critical care, and sleep medicine at the University of Cincinnati (UC) Medical Center, and Dr. Woods is director, center for pulmonary imaging research, Cincinnati Children’s Hospital Medical Center.
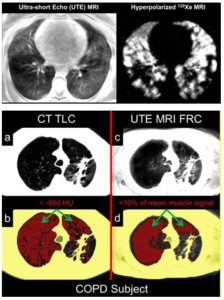
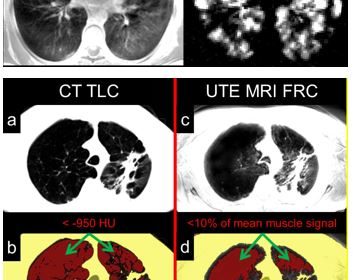
These images from a rare-lung patient (top) and a COPD patient (middle, bottom) demonstrate the ability of MRI to depict and quantify 1) regional ventilation, 2) high-resolution parenchyma, and 3) pathologies very similar to CT scanning. Images courtesy of Frank McCormack, MD
The novel MRIs available on the campus have three forms: proton MRI, with an ultrashort echo time that produces high resolution images compared to traditional MRI, also known as UTE MRI, and two hyperpolarized gas-MRIs: 3He (a rare isotope in short supply used in adults for research purposes in the last 15 years) and 129Xe (less expensive than 3He and more commonly used recently). With 129Xe, real-time ventilation can be depicted, and alveolar size and gas exchange can be quantified.
Drs. McCormack and Woods describe how the use of MRI could be advantageous in patients who need serial scanning, whether for clinical or research purposes. According to Dr. McCormack, “CT has been considered the gold standard for imaging the lung, but repeat CTs pose the risk of cumulative radiation exposure.” Dr. Woods points out that “MRIs are non-ionizing and can be used to serially image patients over time without being concerned about increased radiation dosage.” The resolution of UTE MRI has been steadily improving, and trials to determine utility in pulmonary fibrosis and obstructive lung diseases are underway. Novel applications of MRI scanning in patients at UC Medical Center3 have included studies of COPD, bronchopulmonary dysplasia, congenital diaphragmatic hernia and cystic fibrosis.4,5 Hyperpolarized gas MRI can detect regional airflow obstruction and responses to treatment in ways that are not possible with pulmonary function tests,6” says Dr. McCormack.
Drs. McCormack and Woods are involved in both adult and pediatric MRI studies. “MRI is being studied in trials of early treatment of lymphangioleiomyomatosis (LAM), a cystic lung disease that affects young women, as a means to identify the earliest signs of lung involvement,7” notes Dr. McCormack. In children, Dr. Woods says, “we’ve been able to quantitatively and qualitatively characterize pulmonary abnormalities in some pediatric conditions for the first time.” In particular, “we’re are filling gaps in knowledge for chronic lung diseases of prematurity that have previously been a black box,” Dr. Woods says. In the neonatal ICU, a novel, tiny MRI device was invented to image the chest for the characterization of pathological changes, as well as to position feeding tubes in a manner that poses no radiation risk.
Together, the UC Medical Center and Cincinnati Children’s Hospital Medical Center campus is one of seven sites worldwide studying hyperpolarized gas-MRIs, and is the hub of the 129Xe MRI Clinical Trials Consortium, which is beginning to design multi-site MRI studies in a variety of obstructive lung diseases.
References
1. RP Thomen, JD Quirk, DA Roach, K Ruppert, T Altes, RW Yusen, T Egan-Rojas, DA Yablonskiy, JC Woods, Direct comparison of 129Xe diffusion measurements with quantitative histology in human lungs, Magn Reson Med 2015, 2016 Jan 17. doi: 10.1002/mrm.26120.
2. RP Thomen, LL Walkup, DJ Roach, ZI Cleveland, JP Clancy, JC Woods, Hyperpolarized 129Xe for investigation of mild cystic fibrosis lung disease in pediatrics, J Cyst Fibr 2016, Jul 28. pii: S1569-1993(16)30565-3. doi: 10.1016/j.jcf.2016.07.008
3. Roach DJ, Crémillieux Y, Serai SD, Thomen RP, Wang H, Zou Y, Benzaquen S, Szczesniak RD, Woods JC. Morphological and quantitative evaluation of emphysema in COPD patients: a comparative study of MRI with HRCT. J Magn Reson imag. 2016, in press.
4. Walkup LL, Thomen RP, Akinyi T, Watters E, Ruppert K, Clancy JP, Woods JC, Cleveland ZI. Feasibility, tolerability, and safety of pediatric hyperpolarized 129Xe magnetic resonance imaging in healthy volunteers and subjects with cystic fibrosis. Pediatr Radiol. 2016, in press.
5. Higano NS, Hahn AD, Tkach JA, Cao X, Walkup LL, Thomen RP, Merhar SL, Kingma PS, Fain SB, Woods JC. Retrospective respiratory self-gating and removal of bulk motion in pulmonary UTE MRI of neonates and adults. Magn Rson Med. 2016 Mar 12. doi: 10.1002/mrm.26212. [Epub ahead of print]
6. Thomen RP, Walkup LL, Roach DJ, Cleveland ZI, Clancy JP, Woods JC, Hyperpolarized 129Xe for investigation of mild cystic fibrosis lung disease in pediatric patients. J Cyst Fibros. 2016 Jul 28. pii: S1569-1993(16)30565-3.
7. McCormack FX, Travis WD, Colby TV, Henske EP, Moss J. Lymphangioleiomyomatosis Calling it what it is: a low-grade, destructive metastasizing neoplasm. Am J Respir Crit Care Med. 2012;186:1210-1212.
Additional reading
JD Quirk, AL Sukstanskii, JC Woods, BA Lutey, MS Conradi, DS Gierada, M Castro, DA Yablonskiy. Experimental evidence of age-related adaptive changes in human acinar airways. J Appl Physiol. 2016;120:159-165. PMID 26542518.
Thomen RP, Quirk JD, Roach DA, Ruppert K, Altes T, Yusen RW, Egan-Rojas T, Yablonskiy DA, Woods JC. Direct comparison of 129Xe diffusion measurements with quantitative histology in human lungs. Magn Reson Med. 2016 Jan 17. doi: 10.1002/mrm.26120. [Epub ahead of print, PMID 26778748]
Thomen RP, Sheshadri A, Quirk JD, Kozlowski J, Ellison HD, Szczesniak RD, Castro M, Woods JC. Regional ventilation changes in severe asthma after bronchial thermoplasty with 3He MR imaging and CT. Radiology. 2015; 274:250-259. PMID 25144646.
Pennati F, Quirk JD, Yablonskiy DA, Castro M, Aliverti A, Woods JC. Assessment of regional lung function by multi-volume 1H-MRI in health and obstructive lung disease: comparison with 3He-MRI. Radiology. 2014; 273:580-590.
 Francis McCormack, MD
Francis McCormack, MD
Taylor Professor and Director, Division of Pulmonary, Critical Care & Sleep Medicine
Professor of Medicine
PHONE: 513-484-5697
EMAIL: frank.mccormack@uc.edu
Connect with Dr. McCormack on Doximity
 Jason Woods, PhD
Jason Woods, PhD
Director, Center of Pulmonary Imaging Research, Cincinnati Children’s Hospital Medical Center
PHONE: 513-803-4463
EMAIL: jason.woods@cchmc.org

