Groundbreaking Research into Rare Lung Disease Pulmonary Alveolar Microlithiasis
The National Heart, Lung, and Blood Institute has awarded an R01 grant of nearly $1.6 million to a team of University of Cincinnati (UC) researchers to study the unusual lung disease, pulmonary alveolar microlithiasis (PAM). The study’s principal investigator is Francis X. McCormack, MD, Director of the Division of Pulmonary, Critical Care and Sleep Medicine at the University of Cincinnati Medical Center. McCormack and his team hope that this study will lead to new biomarkers and treatment approaches for the ultra-rare disease. In addition, the animal model they have developed is yielding surprising new insights into the fundamental biology of the lung.
The Science of PAM
PAM is caused by inactivating mutations in the SCL34A2 gene.1 The mutation leads to reduced phosphate reuptake by Npt2b sodium phosphate transporter in the apical membrane of type II alveolar cells, resulting in calcium phosphate microlith formation in alveolar spaces.1 The defective genes must be inherited from both parents, and the disease is more likely to occur in areas of the world where intermarriage within families is prevalent. PAM can be diagnosed with characteristic radiological findings, and biopsy is not usually required.1
The Case that Inspired the Study
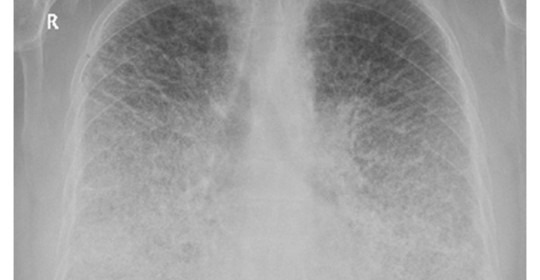
The PAM mouse model study was inspired by a patient seen by Dr. McCormack in 2011 at UC Medical Center. The woman had been diagnosed with PAM as a child in Jordan and developed exertional dyspnea at the age of 54, a typical pattern for PAM. Chest examination revealed bibasilar crackles, pulmonary function tests revealed mild restriction and reduced diffusing capacity, and a six-minute-walk test revealed normal exercise capacity with mild exertional desaturation to 88%.1 Chest X-ray showed fine hyper dense lower lung zone nodular opacities, and computed tomography of the chest showed symmetrical lower lobe predominant micronodular calcifications along bronchovascular bundles and interlobular septal thickening, findings pathognomonic for PAM.1

Chest x-ray of patient with PAM showing hyper dense, fine nodular opacities in the lower lung zones1.
Mouse Model Yields Surprising Results, Leads to Ideas for Trials
The investigators replicated the genetic defect which knocks out the Npt2b transporter in mice, and observed that abundant microliths, or calcifications, formed in the lung. The time dependent accumulation of stones was accompanied by increases in inflammatory proteins in the alveolar lavage and serum of the mice. To explore the relevance of these mouse findings to humans, McCormack’s team collected blood samples from sites participating in the Rare Lung Diseases Consortium in the United States, Croatia, Spain, Turkey and Japan. They found that stone burden correlated with the levels of monocyte chemotactic protein 1 (MCP-1) and surfactant protein D (SP-D) in serum, biomarkers of lung injury and barrier dysfunction, respectively.
Surprisingly, surfactant phospholipid levels were also elevated in the airspaces of the knockout mice, as is known to occur in pulmonary alveolar proteinosis. “These data suggest that phosphate homeostasis may be involved in the regulation of surfactant synthesis or degradation,” says McCormack. If validated, this would be a fundamental new finding in lung biology, stemming from the study of this very rare disease.

Chest computed tomography (CT) of patient with PAM showing symmetrical lower lobe predominant micronodular calcifications along bronchovascular bundles and interlobular septa.
The mouse studies also suggested two ideas for trials. Stones isolated from the lungs of PAM mice readily dissolved in EDTA containing solutions. These data suggest that, if the approach is shown to be safe, therapeutic EDTA lavage could reduce the burden of stones in the lung. In addition, dietary phosphate restriction was shown to prevent microlith deposition and even to reverse established lesions in the lung. These exciting findings were published in the November 11, 2015 edition of the journal Science Translational Medicine.
Trials in humans are planned, but will be challenging for two reasons. First, PAM is exceedingly rare, with just 700 documented cases worldwide since it was discovered in the 1960s. Second, cases are scattered around the globe. Forty cases of PAM have been identified worldwide in the network of pulmonary clinics within the Cincinnati based NIH-grant-funded Rare Lung Disease Consortium, with 16 of those in the United States.
Potential Future Applications
Discoveries made in an orphan disease can shed light on more common disorders. In the case of PAM, McCormack cites the intense interest this rare disease has attracted from researchers in the surfactant and cystic fibrosis fields. “Rapid progress is uniquely possible in the rare diseases,” says McCormack.
Reference: 1. Gupta N and McCormack FX. Images in Pulmonary, Critical Care, Sleep Medicine and the Sciences: Pulmonary Alveolar Microlithiasis. Am J Respir Crit Care Med October 2013. 188(7):e11–e12.
 Francis X. McCormack, MD
Francis X. McCormack, MD
Director, Division of Pulmonary, Critical Care & Sleep Medicine
Professor of Medicine, Department of Internal Medicine
(513) 558-4831 / (513) 475-8523
mccormfx@ucmail.uc.edu
Connect with Francis McCormack, MD on Doximity
Leave a reply →