Endoscopic Lung Volume Reduction Surgery: Transforming the Care of Patients with Severe Emphysema and Pneumothorax
Current surgical approaches to the care of emphysema patients including lung transplantation and lung volume reduction surgery are welcome options for motivated patients who qualify for these advanced procedures, however, many chronic obstructive pulmonary disease (COPD) patients at University of Cincinnati (UC) Medical Center are too ill to be considered. “I am optimistic about the potential for endoscopic lung volume reduction (ELVR), which is approved in other countries and is being trialed in the U.S., to change the standard of care for patients with advanced obstructive lung disease,” says Sadia Benzaquen, MD, assistant professor and director of interventional pulmonology.
Emphysema to Improve Lung Function (EMPROVE) Trial
Dr. Benzaquen heads UC Medical Center’s arm of the trial ‘Evaluation of the Spiration® Valve System for Emphysema to Improve Lung Function (EMPROVE)’. In this multicenter study, participants are randomized to endobronchial valve placement or the control group. Subjects are followed for one, three, and six months, and then annually for five years, or for two years in the medical management group.

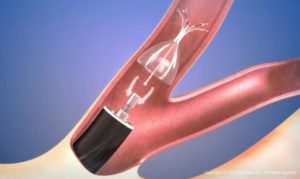
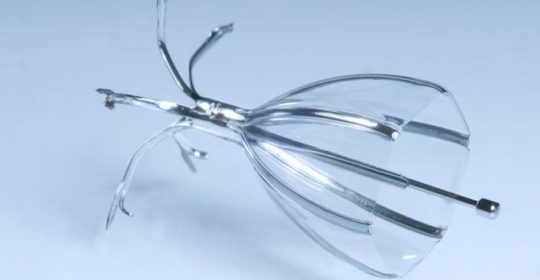
The Spiration Valve is an umbrella-shaped, one-way valve that is placed via a delivery catheter, introduced through the working channel of a flexible bronchoscope. Images courtesy of Spiration, Inc.
The one-way endobronchial valve is an umbrella-like device that is implanted via a bronchoscope into an airway of the most diseased sections of the lung. The valve expands and contracts as the patient breathes, seating itself and creating a tight seal with the airway wall which prevents air from entering the target lobe and, at the same time, permitting the escape of trapped air and fluids. The net result is partial collapse of the hyperinflated lung which restores the curvature of the diaphragm and provides for optimal mechanical advantage. A recent study showed that use of endobronchial valves may result in improved pulmonary function and exercise capacity in patients without interlobar collateral ventilation.1
“The valves are easy to place in the lung and, if necessary, to remove,” says Dr. Benzaquen. “If the EMPROVE trial and other studies are positive, I am confident that placement of these valves will become the standard of care.”
Selecting the Type of ELVR
According to Dr. Benzaquen, the success of ELVR is dependent on two patient characteristics: extent of collateral ventilation between lung segments and heterogeneity in emphysema between regions of the lung. Extensive collateral ventilation is typically an insignificant issue in patients with normal lungs but is present in the majority of patients with severe emphysema. Further, collateral ventilation is present more often in patients with homogeneous emphysema than in those with heterogeneous disease, perhaps explaining why patients with upper lobe predominant disease have better outcomes with ELVR than those with heterogeneous disease.2
Patients with heterogeneous emphysema and a complete fissure (i.e., based on total separation of the upper and lower lobe on CT of the chest by a full length fissure) are candidates for ELVR with valves. Patients with incomplete fissure may be candidates for ELVR with coils, foam, or vapor; emerging approaches to endoscopic lung volume reduction.
Use of Endobronchial Valves for Patients with Pneumothorax
Refractory bronchopleural fistula with pneumothorax is another condition in which the use of endobronchial valves exhibits good patient outcomes, particularly when traditional interventions are unsuccessful. In a 2015 review of 25 case reports and three case series, investigators found that use of endobronchial valves resulted in cessation of a persistent air leak (most commonly due to spontaneous secondary pneumothorax) in less than 24 hours and indicated that their use in high-risk patients, regardless of the cause, should be studied further.4 A 2015 review of 21 patients who underwent 24 valve placements (in total, 88 valves) showed that the use of endobronchial valves was effective in accomplishing removal of chest tubes and hospital discharge in all patients, including 11 with pneumothorax.5 UC Medical Center is one of the few centers in the U.S. participating in the VAST study (valves versus standard of care for the treatment of bronchopleural fistula.
A Summary of Endobronchial Lung Volume Reduction Techniques
In a 2013 review of lung volume reduction choices, Lee and colleagues concluded the following2:
- Valves, the most studied option, can improve lung function and improve quality of life, especially in patients with heterogeneous, upper lobe predominant emphysema without collateral ventilation. They are also easily reversible.
- Biologic lung volume reduction systems, which induce localized inflammation that results in atelectasis by blockage and remodeling, improves lung function. These methods have the advantage that they can be used in patients with homogeneous disease and are not affected by collateral ventilation, but they are not reversible.
- AeriSeal is a variation of the biologic lung volume reduction system. The method uses no human blood products, improves lung function and is not affected by collateral ventilation, but it is irreversible.
- Vapor entails the use of heated water which results in inflammation, followed by permanent fibrosis and atelectasis. This method improves lung function and is not affected by collateral ventilation, but it is irreversible.
- Coils such as the Nitinol coil are deployed as a straight wire in the airway, where they resume their native coiled state and twist and compress surrounding lung tissue. This reduces lung volume and improves lung function without being confounded by collateral ventilation. This method is likely irreversible. More recently, a randomized superiority trial that compared Nitinol coils with usual care in 100 patients at 10 French university hospitals found that use of the coils resulted in improved exercise capacity but significant short-term costs.3
- Airway bypass is based on the placement of stents that establish communication between the large airways and hyperinflated lung segments to decrease trapping of air. This method can be used in patients with homogeneous disease but improvements in early trials were short-term.
References:
1.
- Klooster K, ten Hacken NH, Hartman JE, et al. Endobronchial valves for emphysema without interlobar collateral ventilation.
N Eng J Med
- . 2015;373:2325-2335
2.Lee HJ, Shojaee S, Sterman DH. Endoscopic lung volume reduction. An American perspective. Ann Am Thorac Soc. 2013;10:667-679.
3.Deslée G, Dutau H, Bourdin A, et al, for the REVOLENS Study Group. Lung volume reduction coil treatment vs usual care in patients with severe emphysema: The REVOLENS randomized clinical trial. JAMA. 2016;315:174-184.
4.Gkedkes ID, Mourtarakos S, Gakidis I. Endobronchial valves in treatment of persistent air leaks: a systematic review of clinical evidence. Med Sci Monit. 2015;21:432-438.
5.Reed MF, Gilbert CR, Taylor MD, Toth AW. Endobronchial valves for challenging air leaks. Ann Thorac Surg. 2015;100:1181-1186.
 Sadia Benzaquen, MD
Sadia Benzaquen, MD
Assistant Professor, Department of Internal Medicine
Director of Interventional Pulmonology
University of Cincinnati Medical Center
(513) 475-8523
benzaqsa@ucmail.uc.edu
Connect with Sadia Benzaquen, MD on Doximity
Leave a reply →