At UC Health, we lead the region in scientific discoveries and embrace a spirit of purpose – offering our patients and their families something beyond everyday healthcare. At UC Health, we offer hope.
Performance Voice & Professional Voice
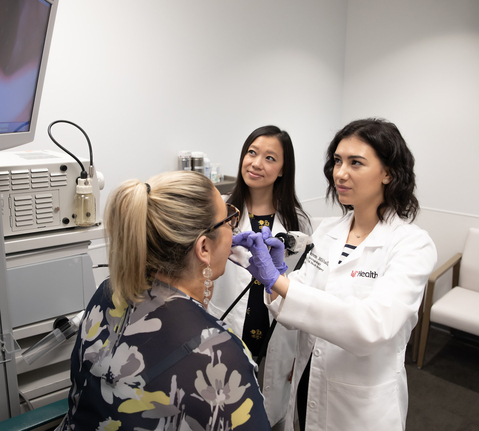
We understand how important your voice is to your life and your career. Our voice subspecialists are highly trained and experienced in treating both urgent and chronic problems with your voice and vocal cords.
Call for more information or to schedule an appointment.
Whether you are an opera singer, choir member, actor, musician or musical theater professional, we can help you with performance voice problems. We also can help you if your profession — such as teaching, coaching, law or preaching — puts great demands on your voice. Our fellowship-trained laryngologists work closely with other specialists — from pulmonology, neurology and family medicine — to deliver effective, comprehensive treatments.
ACTIVE AND VIBRANT RESEARCH
We Are Committed To Advancing Medical Options.
The best medical programs in the world are part of leading-edge research aimed at improving public health and developing new medical treatments. As the Region’s only adult academic medical center, we house vibrant research programs that include ongoing clinical trials, actively initiating studies to bring new therapies and diagnostic tests to patients in Greater Cincinnati and around the world.
We Actively Seek Medical Discoveries.
Nationally and internationally recognized for its research efforts, the University of Cincinnati College of Medicine and UC Health has a long and distinguished history of medical discoveries. Our premier surgeon-scientists and postdoctoral researchers pursue innovative and exciting research, focused on applying their discoveries directly to the bedside to advance patient care.
REFERRING A PATIENT
Our Teams Build Strong Collaborative Partnerships With Referring Providers.
We are committed to providing optimal care to your patient and open communication with you. As a referring physician, we understand that you need to be kept informed on your patient’s progress. That’s why we set up a toolbox to share detailed information about your patient’s health with you.
To refer a patient, call 513-475-8400.
Ear, Nose & Throat Events
World Voice Day: One World, Many Voices Virtual Symposium
Do you consider yourself a “performance voice” user? You may be surprised that you ARE.
Teachers, coaches, lawyers, and broadcasters utilize their “performance” voices on a daily basis - which can cause significant strain on the body and vocal folds.
Attendees will learn:
- How to care, protect and celebrate your voice.
- Perspectives from the clinician, physician, teacher, performer, and director
- The importance of vocal health, especially those
- within professional and performance voice-related fields.
- How to train your body and your voice for optimal performance.
- Communication strategies and voice protection for mask users.

Conditions We Treat
Expertise in Treating Common to the Most Complex Conditions
- Chronic Laryngitis
- Laryngopharyngeal Acid Reflux (LPR)
- Muscle Tension Dysphonia (MTD)
- Sulcus Vocalis
- Vocal Fold Bowing
- Vocal Fold Cysts
- Vocal Fold Hemorrhage
- Vocal Fold Nodules
- Vocal Fold Polyps
- Vocal Fold Process Granuloma
- Vocal Fold Pseudocyst
- Vocal Fold Scar
Expert Therapies and Treatments for Voice Conditions
Our voice doctors work with other specialists to deliver hope for complex cases, including patients who haven’t been able to use their voice properly in years.
Advanced Diagnostics & Treatments
Professional Singers Choose Us
The Region’s Only Performance Voice Subspecialists
As the preferred providers for singers at the Cincinnati Opera and the UC College Conservatory of Music, professionals choose us because we offer the most current and comprehensive approaches to voice conditions in the Midwest.

Our Unique Approach
Therapies for Many Voice Issues
Therapy is an important tool in healing your voice, no matter how you use it. We offer a wide variety of voice therapies to meet the needs of your profession and the challenges your voice faces. Our certified speech-language pathologists specialize in training your voice with vocal exercises tailored to each person’s needs and personal goals.
AUTHORING BREAKTHROUGHS
Combining Expertise with Advanced Care
Performance and Professional Voice
Our voice subspecialists help with every voice issue, from performance singers and actors, to professional teachers, broadcasters, lawyers and preachers.
Community Support
Our team of experts offers community outreach to choirs, schools and support groups including transgender and Parkinson’s disease.
4 Convenient Locations
With your busy schedule, we make it easy to find treatment. Patients all over the Midwest choose our convenient Greater Cincinnati locations.
Our Providers
No physicians found.
HOW YOU CAN CONTRIBUTE
Donations from people like you make the difference.
By advancing medicine, our life-changing research and treatments help countless patients here and around the world. Please donate today.