A Genetic Variant Can Predispose South Asians to Hypertrophic Cardiomyopathy
A genetic variant of myosin binding protein C, cardiac (MYBPC3), can predispose South Asians to hypertrophic cardiomyopathy (HCM), but early screening could lower its incidence. Sakthivel Sadayappan, PhD, MBA, professor, division of cardiovascular health and disease and director of the heart branch of Heart, Lung and Vascular Institute, University of Cincinnati Medical Center (UC Medical Center), is one of the researchers who discovered the genetic variant1. Dr. Sadayappan and his colleagues are trying to determine if cardiac (MYBPC3) is pathogenic or a modifier that causes HCM; and if it is pathogenic, identifying the mechanism.
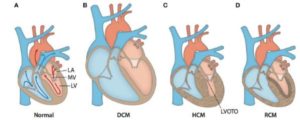
Anatomical cross-sections of hearts with various forms of cardiomyopathy. (A) Arrows outline the path of blood flow in a healthy heart. Blue corresponds to the deoxygenated venous return to the heart. Red corresponds to the oxygenated blood in the left side of the heart. After oxygen saturation in the lungs, blood is directed from the left atrium (LA) through the mitral valve (MV) into the left ventricle (LV). Then, it is pumped through the aorta to the rest of the body. (B) A typical enlarged heart seen in DCM, with thin and stretched walls and large chamber volumes. (C) A typical heart seen in HCM, with generalized hypertrophy and reduced size of the LV chamber. Increased wall thickness of the interventricular septum and protrusion of the MV into the outflow path contribute to left ventricular outflow tract obstruction (LVOTO). (D) A typical heart seen in RCM with ventricular walls of normally thickness. The walls are stiffened by increased fibrotic deposition, which is signified by darker shading.
Dr. Sadayappan described cardiac (MYBPC3) as no respecter of caste or gender, given its frequent appearance in 1.8 billion South Asians, 22 million of whom live outside South Asia.2 In the United States, South Asians (4 million people, or 1% of the US population)2 have been found to have an almost 50% greater mortality rate from cardiovascular disease compared with other ethnic groups.3 Further, 4% to 5% of South Asians carry the genetic variant, cardiac (MYBPC3), the gene most frequently associated with HCM, which can result in heart failure and sudden cardiac death4 (South Asian countries consist of: Afghanistan, Bangladesh, India, Nepal, Pakistan, and Sri Lanka).
Dr. Sadayappan and his lab are currently involved in a research project named the Diastolic Dysfunction of South Asians (DOSA) study, which is an American Heart Association Cardiovascular Genome Phenome Study. Its goal is to define the evidence of diastolic dysfunction in South Asian subjects who carry the (MYBPC3) variant and live in the United States. Dr. Sadayappan presented the results of this study with a poster session titled, “A Polymorphic (MYBPC3) Variant as a Major Risk Factor of Cardiomyopathy in South Asian Descendants,” at the annual American Heart Association meeting in November 2016. The presentation detailed a screening study of 2,244 individuals in which Dr. Sadayappan and his associates found that 136 people carried the genetic variant cardiac (MYBPC3). Dr. Sadayappan explained that the screening process begins with collecting blood and saliva samples; those subjects whose samples are found to be positive with respective negative controls are asked to come to the hospital for an echocardiography and electrocardiogram, and additional urine and blood samples. In addition to looking for cardiac (MYBPC3), “we also look for the presence of diabetes and hypertension, which increase the odds of developing cardiomyopathy,” he said.
With an NIH grant, Dr. Sadayappan is studying transgenic mouse models to define the molecular mechanism of the South Asian-specific (MYBPC3) variant. Not all of his work is associated with disease pre-deposition; he and his associates are also studying the structure and the function of cardiac proteins with the help of two NIH grants.
Given the individual nature of HCM’s genetic variants and clinical phenotypes, the development of more personalized medicine is expected to result in more person-specific treatments for HCM. The 2015 Precision Medicine Initiative is aimed at individualizing healthcare, from diagnosis of illnesses and conditions to delivery of treatments.2 The Sarcomeric Human Cardiomyopathy Registry (SHaRe) brings together geneticists and cardiologists from the United States and Europe to discuss and develop long-term data about HCM and dilated cardiomyopathy. Established in 2014 with the help of MyoKardia, the registry de-identified data on approximately10,000 subjects with the goal of trying to develop precision medicines. According to Dr. Sadayappan, a Phase I clinical trial will begin soon at UC Medical Center.2,5
References
1 Waldmüller S, Sadayappan S, Vahab Saadi A, Selignow C, Gopal Rakesh P, Golubenko M., … Vosberg, H.P. Novel deletions in MYH7 and MYBPC3 identified in Indian families with familial hypertrophic cardiomyopathy. J Mol Cell Cardiol. 2003;35(6): 623–636.
2. Kraker J, Viswanathan SK, Knöll R, Sadayappan, S. Recent advances in the molecular genetics of familial hypertrophic cardiomyopathy in South Asian descendants. Front Physiol. 2016;7:499.
3. Klatsky AL, Tekawa I, Armstrong MA, Sidney S. The risk of hospitalization for ischemic heart disease among Asian Americans in northern California. Am J Public Health. 1994;84:1672-1675.
4. Barefield D, Sadayappan S. Phosphorylation and function of cardiac myosin binding protein-C in health and disease. J Mol Cell Cardiol. 2010;285(8):5674-5682.
5. MyoKardia ShaRe Registry. Available at http://www.myokardia.com/patientsShare.php. Accessed December 22, 2016.
Additional Reading
Barefield DY, Lynch TL IV, Jagadeesan A, Sanagala T, Sadayappan S. High-throughput diagnostic assay for a highly prevalent cardiomyopathy-associated MYBPC3 variant. J Mol Biomark Diagn. 2016;7:6.
Sakthivel Sadayappan, PhD, MBA
Professor, Department of Internal Medicine Division of Cardiovascular Health and Disease
Director, Heart Branch of the UC Heart, Lung and Vascular Institute
PHONE: (513) 558-7498
E-MAIL: sadayasl@uc.edu


