At the University of Cincinnati Cancer Center, we lead the region in scientific discoveries and embrace a spirit of purpose – offering our patients and their families something beyond everyday healthcare. At the University of Cincinnati Cancer Center, we offer hope.
Genitourinary Cancer Center
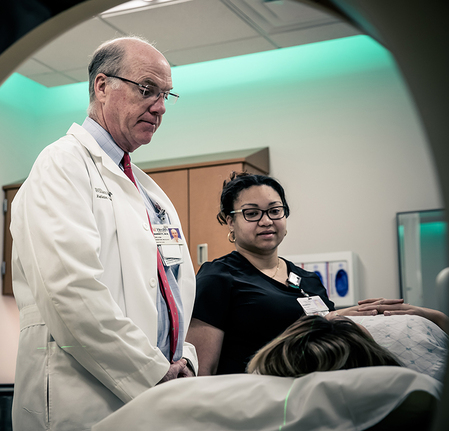
Our expert team of physicians and researchers pledge their knowledge and experience to help you during your treatment and recovery from genitourinary cancer.
Call for more information or to schedule an appointment.
We understand that a cancer diagnosis can be frightening. We’re here to help you find the right treatment and navigate the many resources available to support you. Our genitourinary cancer team subspecializes in treating all stages of prostate, kidney, bladder, adrenal and testicular cancers. We’re focused on delivering the latest in medical breakthroughs. Our team of highly trained experts promise to never stop seeking what’s next.
ACTIVE AND VIBRANT RESEARCH
We Are Committed To Advancing Medical Options.
The best medical programs in the world are part of leading-edge research aimed at improving public health and developing new medical treatments. As the Region’s only adult academic medical center, we house vibrant research programs that include ongoing clinical trials, actively initiating studies to bring new therapies and diagnostic tests to patients in Greater Cincinnati and around the world.
We Actively Seek Medical Discoveries.
Nationally and internationally recognized for its research efforts, the University of Cincinnati College of Medicine and UC Health has a long and distinguished history of medical discoveries. Our premier surgeon-scientists and postdoctoral researchers pursue innovative and exciting research, focused on applying their discoveries directly to the bedside to advance patient care.
REFERRING A PATIENT
Our Teams Build Strong Collaborative Partnerships With Referring Providers.
We are committed to providing optimal care to your patient and open communication with you. As a referring physician, we understand that you need to be kept informed of your patient’s progress. That’s why we set up a toolbox to share detailed information about your patient’s health with you.
To refer a patient, call 513-585-UCCC.

Conditions We Treat
With research and experience, we’re helping patients like you overcome genitourinary cancers every day.
Leading-Edge Treatments for Genitourinary Cancers
Your health deserves both world-renowned experts and the support system you can only find at home in Greater Cincinnati. With UC Health, you’ll find both.
Advanced Diagnostics & Treatments
YOUR PERSONALIZED CARE TEAM
Compassionate Care, Top-Notch Treatment
Every patient and every cancer is unique, so we focus on providing the best treatments at the right time. We help you understand your diagnosis, your treatment options and your prognosis.
AUTHORING BREAKTHROUGHS
Nationally Recognized for Superior Care
Better Diagnosis, Better Treatment
We have the most experience in the region to use MRI/ultrasound fusion technology, which helps diagnose and treat prostate cancer patients more effectively.
Kidney Cancer Treatment
Only team in the region offering robotic surgery for complex multifocal kidney cancer and leading-edge treatments for metastatic kidney cancer through clinical trials.
Multidisciplinary Prostate Cancer Clinic
The first of its kind in the region, our clinic educates prostate cancer patients about treatment options so you can determine what is best for you.

Patient Stories
Precise Procedures For Prostate Cancer
Two Patients; Two Treatments; Two Success Stories
Our Providers
No physicians found.
HOW YOU CAN CONTRIBUTE
Donations from people like you make the difference.
By advancing medicine, our life-changing research and treatments help countless patients here and around the world. Please donate today.